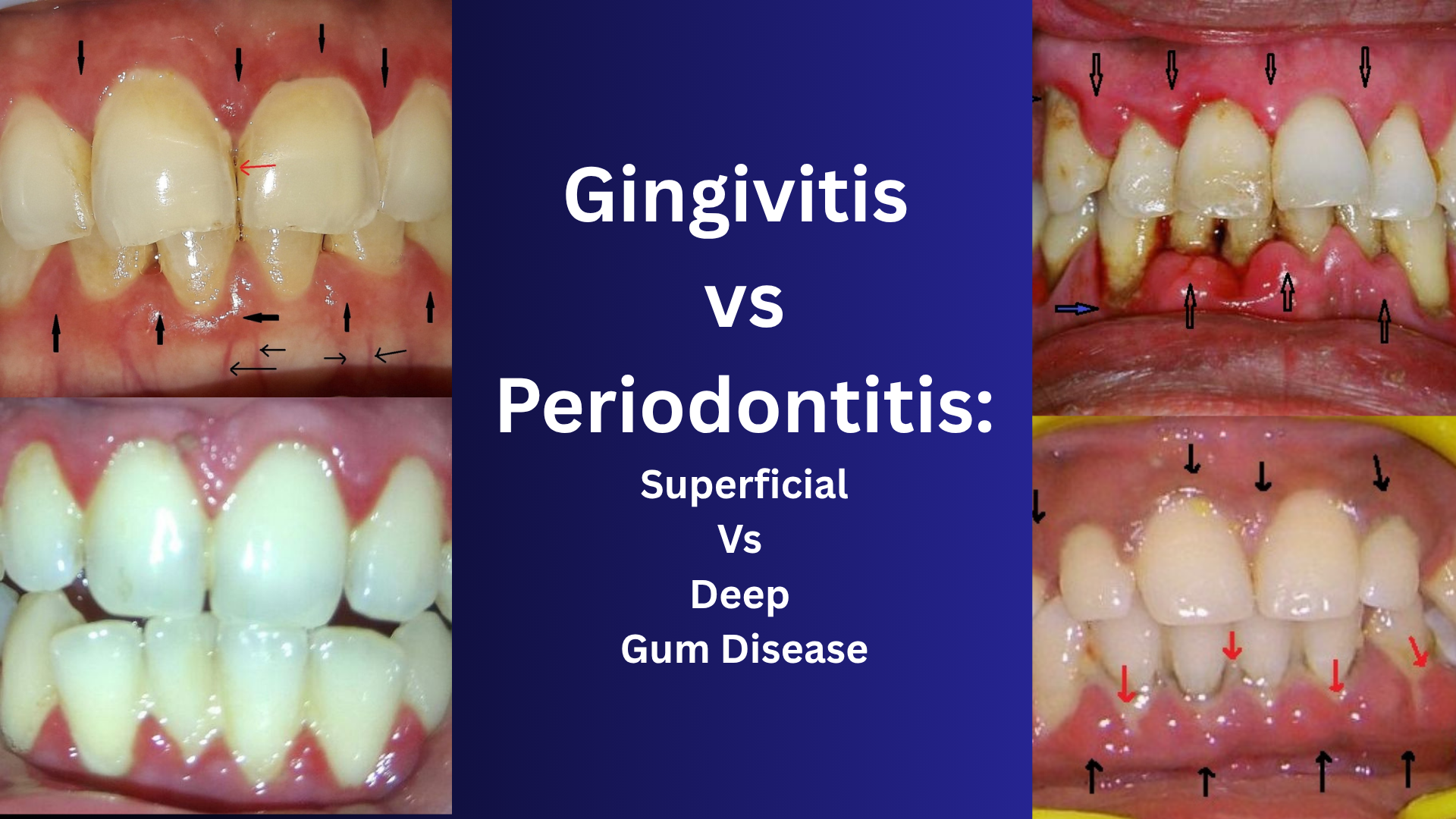
Gingivitis vs Periodontitis
Introduction: Understanding the Health of Your Gums
Gum disease doesn’t just affect your mouth—it can impact your entire well-being. Two of the most common forms of gum disease are gingivitis and periodontitis. While they may seem similar, they differ drastically in severity, causes, symptoms, and treatment. Gingivitis is often mild and reversible, whereas periodontitis is more serious and can lead to tooth loss if untreated. In this detailed guide, we break down these two conditions in a simple, layperson-friendly way, covering all ultra-nano aspects under the topic.
What Is Gingivitis? (Superficial Gum Disease)
Definition:
Gingivitis is the early, mild stage of gum disease. It involves inflammation of the gums without affecting the bone or deeper structures that support the teeth.
Key Causes:
- Poor oral hygiene
- Plaque buildup
- Hormonal changes (puberty, pregnancy, menopause)
- Certain medications
- Smoking
- Diabetes
- Nutritional deficiencies (Vitamin C)
Signs and Symptoms:
- Red, swollen gums
- Bleeding while brushing or flossing
- Tenderness in the gums
- Bad breath (halitosis)
- Mild gum recession (sometimes)
Is Gingivitis Reversible?
Yes. With proper oral care and professional cleaning, gingivitis can be completely reversed.
Treatment Options:
- Professional dental cleaning (scaling)
- Improved brushing and flossing habits
- Antibacterial mouthwash
- Lifestyle changes (quitting smoking, managing diabetes)
- Regular dental checkups
What Is Periodontitis? (Deep Gum Disease)
Definition:
Periodontitis is the advanced, destructive stage of gum disease. It starts as untreated gingivitis and spreads below the gum line, causing damage to the bone and ligaments that support your teeth.
Types of Periodontitis:
- Chronic Periodontitis (most common)
- Aggressive Periodontitis (faster bone loss, often in younger people)
- Necrotizing Periodontitis (associated with immune conditions like HIV)
- Periodontitis as a Manifestation of Systemic Diseases (e.g., diabetes)
Causes and Risk Factors:
- Long-standing plaque and tartar
- Genetics
- Uncontrolled diabetes
- Smoking
- Poor nutrition
- Certain systemic diseases
- Stress (affecting immune response)
Signs and Symptoms:
- Persistent bad breath
- Deep gum pockets
- Loose or shifting teeth
- Pain while chewing
- Pus between gums and teeth
- Receding gums
- Tooth sensitivity
Is Periodontitis Reversible?
No. The damage caused by periodontitis cannot be fully reversed, but it can be controlled and managed with timely treatment.
Treatment Options:
- Scaling and Root Planing (deep cleaning)
- Gum Surgery (flap surgery, bone grafting)
- Laser Therapy
- Antibiotics (topical or systemic)
- Periodontal maintenance every 3–4 months
Comparison Table: Gingivitis vs Periodontitis
| Feature | Gingivitis | Periodontitis |
| Severity | Mild | Moderate to severe |
| Reversibility | Yes | No (only manageable) |
| Affected Tissues | Gums only | Gums, bone, ligaments |
| Symptoms | Swollen, bleeding gums | Loose teeth, gum pockets, bone loss |
| Treatment | Oral hygiene, cleaning | Deep cleaning, surgery, antibiotics |
| Pain | Usually painless | Often painful |
Gum Disease Progression Timeline (If Untreated)
- Plaque Formation →
- Gingivitis (reversible) →
- Early Periodontitis (mild bone loss) →
- Moderate Periodontitis (pocket formation, gum recession) →
- Advanced Periodontitis (tooth mobility, bone destruction, tooth loss)
Why Early Detection Matters
- Cost-effective: Gingivitis treatment is simpler and less expensive.
- Prevents complications: Periodontitis is linked to heart disease, diabetes, and low birth weight in pregnancy.
- Saves teeth: Early care can help retain your natural smile for life.
Home Care Tips for Healthy Gums
- Brush twice daily with a soft-bristle toothbrush
- Use fluoride toothpaste
- Floss once daily
- Use an antimicrobial or fluoride mouthwash
- Quit smoking
- Eat a balanced diet
- Get dental checkups every 6 months
When to See a Dentist Immediately
- Bleeding gums that persist
- Loose or shifting teeth
- Gum abscess (pus, swelling)
- Pain while chewing
- Bad breath that doesn’t go away
10 FAQs Not Covered in the Article
- Can gingivitis come back after treatment?
Yes, especially if oral hygiene is not maintained. - Can children get gingivitis or periodontitis?
Children can get gingivitis, but periodontitis is rare in kids unless there’s a genetic or systemic factor. - Is gum disease contagious?
Gum disease is not directly contagious, but bacteria can be shared through saliva. - Can mouthwash alone cure gingivitis?
No. Mouthwash is supportive but not a standalone treatment. - Is gum bleeding normal?
No. Bleeding gums are usually a sign of inflammation. - Does pregnancy worsen gum disease?
Yes, due to hormonal changes, pregnant women are more prone to gingivitis. - Can gum disease be cured naturally?
Natural remedies can help reduce symptoms but cannot replace professional treatment. - How often should periodontal patients get cleanings?
Every 3–4 months for maintenance. - Can I get dental implants if I had periodontitis?
Yes, if the infection is well-controlled and bone levels are adequate. - Are electric toothbrushes better for gum disease?
Yes, many studies support their superior plaque removal ability.
Call to Action
Explore our Gum Care Shop for essential products that support healthy gums and lasting oral hygiene.
Bleeding Gums & Gum Disease Related Reads
Gum Disease: Everything You Need to Know
Gum Pigmentation: Harmless or a Hidden Health Warning?
Can Gum Disease Be Reversed? Realistic Expectations & Proven Timeline for Recovery
Bleeding Gums in Pregnancy – Causes, Prevention & Safe Home Care for Moms-to-Be
How Smoking Affects Your Gums – The Silent Damage You Can’t Ignore
Gum Disease in Diabetics – What You Need to Know
How Stress Affects Gum Health – The Hidden Mind-Body Connection You Can’t Ignore
How Long Does Gum Treatment Take? A Complete Step-by-Step Timeline for Healthier Gums
Gum Surgery Cost Explained: Country-wise & City-wise Comparison (USA, UK, India, China)