Lichen planus is a chronic autoimmune disorder that can affect the skin, mucous membranes, nails, and hair. When it involves the mouth, it is termed oral lichen planus (OLP), which is considered a precancerous condition due to its potential to increase the risk of oral cancer, particularly in its erosive or atrophic forms. In some cases, lichen planus may affect only the skin, only the mucosa (including the mouth or other mucosal areas), or both. The condition is non-contagious but has the potential to persist for long periods, significantly impacting the quality of life.
This article provides a detailed look at lichen planus, its oral and skin presentations, potential visceral organ involvement, and the steps for managing and preventing its complications.
What Is Lichen Planus?
Lichen planus is an autoimmune disease where the immune system mistakenly attacks the cells of the skin and mucosa. It typically presents as itchy, flat-topped purple papules on the skin or lace-like white patches in the oral cavity. The condition may also involve other mucosal sites like the genitals, esophagus, and conjunctiva.
In some instances, lichen planus affects visceral organs, although this is rare. Esophageal lichen planus can cause strictures or difficulty swallowing, and there have been isolated reports of involvement of the gastrointestinal and urogenital tracts.
Features of Lichen Planus
Skin Features
- Flat-Topped Purple Papules: Small, shiny, polygonal bumps, often with a purple hue.
- Itching: A hallmark symptom that often drives patients to seek medical care.
- Koebner Phenomenon: Lesions may appear at sites of trauma or injury.
- Commonly Affected Areas:
- Wrists and forearms
- Ankles and legs
- Lower back
- Scalp and Nail Involvement: Can cause hair thinning or scarring alopecia and nail ridging or thinning in some cases.
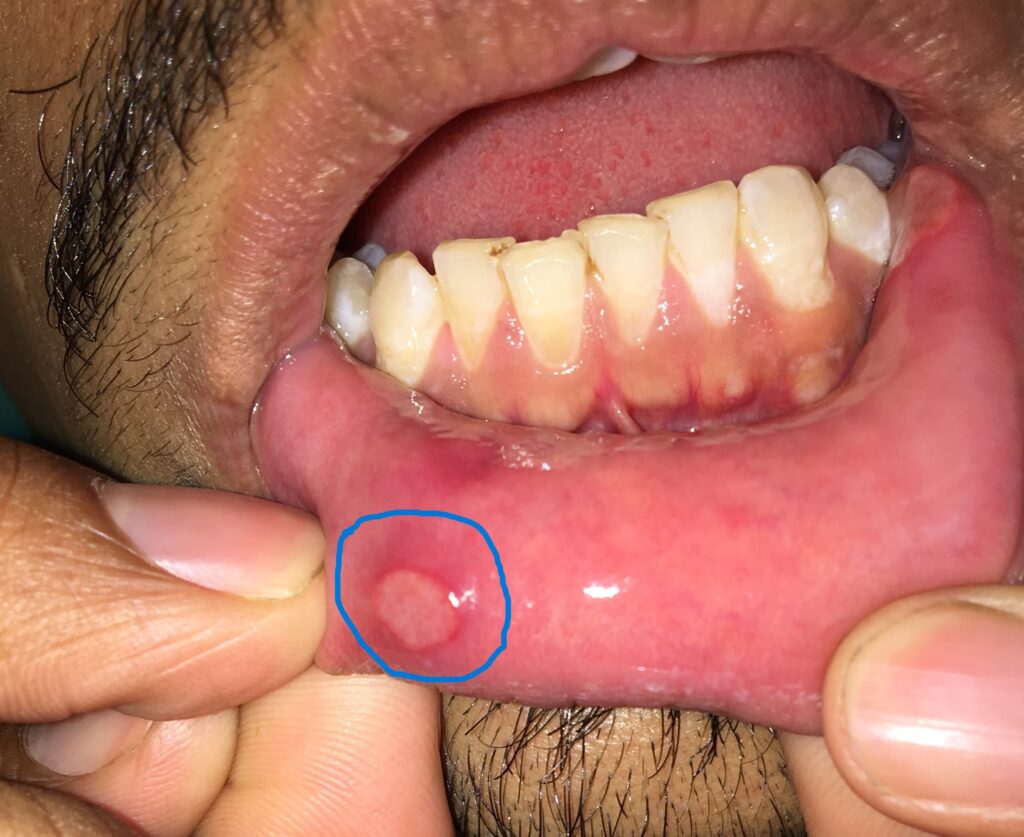
Oral Features
- White, Lace-Like Patches: Also known as Wickham’s striae, these are the most common oral manifestation.
- Red, Inflamed Lesions: These may develop into painful ulcers.
- Burning Sensation: Often exacerbated by spicy, acidic, or hot foods.
- Sites Involved: Inner cheeks, tongue, gums, lips, and occasionally the palate.

Oral lichen planus
Other Mucosal Sites
- Genital Mucosa: Can cause pain, irritation, or white patches in the genital area.
- Esophagus: May lead to swallowing difficulties in severe cases.
- Conjunctiva: Rarely, lichen planus may affect the eyes.
Types of Lichen Planus
- Cutaneous Lichen Planus: Affects only the skin.
- Oral Lichen Planus: Limited to the oral mucosa.
- Mucocutaneous Lichen Planus: Affects both skin and mucosal surfaces.
- Hypertrophic Lichen Planus: Thickened, scaly lesions primarily on the lower legs.
- Erosive Lichen Planus: Painful erosions or ulcers in the mouth or other mucosal areas, with a higher risk of malignant transformation.
Causes of Lichen Planus
The exact cause of lichen planus remains unknown, but it is believed to involve an autoimmune mechanism. Factors that may contribute include:
- Genetic Predisposition: Family history of autoimmune diseases.
- Triggers: Stress, trauma, or irritants.
- Lifestyle Factors: Smoking and alcohol use can aggravate the condition and increase the risk of complications.
- Medications: Certain drugs (e.g., NSAIDs, antihypertensives) may induce a lichen planus-like reaction.
Does Lichen Planus Affect Visceral Organs?
While primarily a disease of the skin and mucosa, lichen planus can rarely involve visceral organs, most commonly the esophagus. Esophageal lichen planus may present with difficulty swallowing, strictures, or discomfort and requires specialized care.
Prevention of Lichen Planus
Although lichen planus cannot always be prevented, certain steps can minimize its severity or frequency of flare-ups:
- Quit Smoking and Alcohol: These habits exacerbate symptoms and may increase the risk of malignant transformation.
- Stress Management: Stress can trigger or worsen the condition; consider mindfulness, yoga, or therapy.
- Gentle Oral Hygiene: Use mild toothpaste and avoid harsh mouthwashes to prevent irritation.
- Dietary Modifications: Avoid spicy, acidic, or hot foods that can irritate lesions.
- Protect Your Skin: Minimize trauma to the skin, which can trigger new lesions (Koebner phenomenon).
Self-Screening for Lichen Planus
Self-screening can help in the early identification of symptoms:
- Check Skin and Mouth Regularly: Look for purple papules on the skin or white patches in the mouth.
- Monitor Itching: Persistent itching warrants medical attention.
- Note Pain or Burning: Especially in the mouth or during eating.
- Inspect Other Areas: Check for lesions on genital mucosa or difficulty swallowing.
If you notice persistent symptoms, consult a healthcare provider for a thorough evaluation.
Treatment Options for Lichen Planus
Consult a specialist for oral lichen planus: an oral physician or dentist for oral lesions and a dermatologist for skin involvement. Patients should avoid self-treatment, as improper management can lead to serious consequences.
Treatment focuses on relieving symptoms, reducing inflammation, and preventing complications.
-
Medical Management
- Corticosteroids: Topical or systemic steroids to manage inflammation.
- Immunosuppressants: Tacrolimus or cyclosporine for severe cases.
- Antihistamines: To reduce itching on the skin.
- Analgesics: Pain-relieving gels for oral lesions.
-
Lifestyle Adjustments
- Avoid smoking and alcohol to prevent symptom aggravation.
- Maintain a healthy diet to support immune function.
-
Regular Monitoring
Patients with lichen planus, especially the erosive type, should undergo periodic screenings for early detection of malignant transformation.
Conclusion
Lichen planus is a multifaceted condition that affects the skin, mucosa, and sometimes visceral organs. While it is not contagious, the chronic nature and potential complications warrant careful management. By adopting healthy habits and seeking timely treatment, patients can significantly improve their quality of life and reduce the risk of malignant transformation.
Q&A: Common Questions About Lichen Planus
Q: Is lichen planus contagious?
A: No, lichen planus is an autoimmune condition and cannot be transmitted to others.
Q: Can lichen planus affect internal organs?
A: Rarely, lichen planus may involve the esophagus or other mucosal sites, leading to symptoms like difficulty swallowing.
Q: Is oral lichen planus painful?
A: Erosive or ulcerative forms of oral lichen planus can cause significant pain or burning, especially while eating.
Q: How is lichen planus diagnosed?
A: Diagnosis is made through clinical examination, and in some cases, a biopsy may be performed to confirm the condition.
Q: Can lichen planus turn into cancer?
A: While rare, chronic lichen planus (especially erosive types) carries a small risk of malignant transformation into squamous cell carcinoma.