Gum Disease and Diabetes.
Introduction
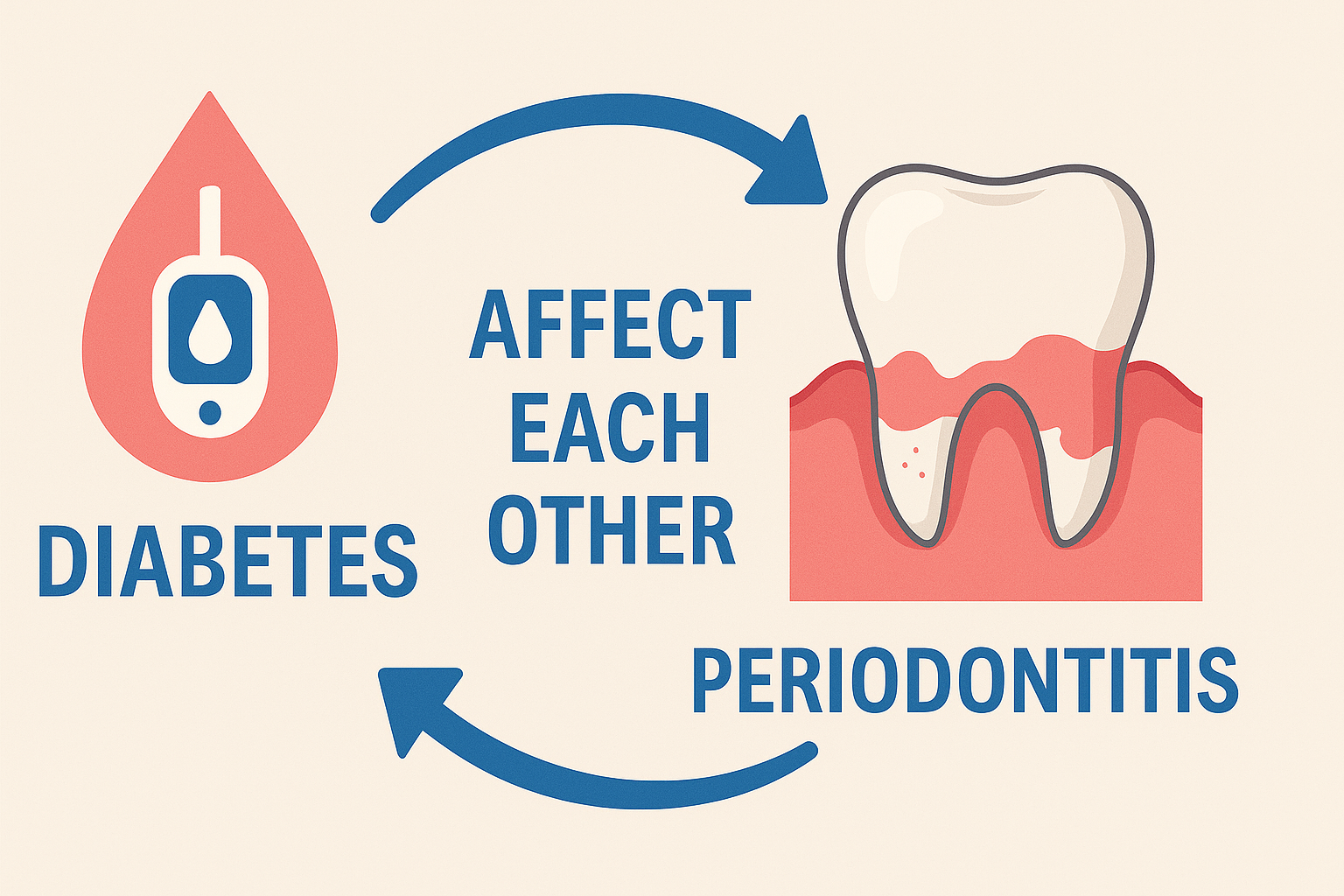
The relationship between gum disease and diabetes is not just a coincidence — it’s a scientifically proven two-way street. Gum disease (also known as periodontal disease) can make blood sugar levels harder to control, and diabetes can worsen gum health, even in people with minimal plaque buildup.
People with diabetes are more likely to develop gingivitis (early gum disease) and periodontitis (advanced gum disease). What’s more alarming is that even mild gum infections can progress rapidly in diabetics, due to changes in immunity, blood flow, and healing capacity. In some severe diabetes cases, gum damage can occur without any bacterial infection, purely from the metabolic effects of the disease itself.
This article explains the deep connection between gum disease and diabetes, the mechanisms behind it, and how to protect both your oral and general health.
🦷 What is Gum Disease?
Gum disease is an inflammatory condition of the supporting structures of the teeth — gums, periodontal ligament, and jawbone. It develops in two stages:
- Gingivitis – Red, swollen gums that bleed easily.
- Periodontitis – Destruction of gums, ligaments, and bone, leading to loose teeth and possible tooth loss.
🔄 The Two-Way Link Between Gum Disease and Diabetes
- How Diabetes Increases Gum Disease Risk
Diabetes affects periodontal health in two main ways:
- Indirectly — By Lowering Immunity & Blood Flow
- Reduced immunity: High blood sugar weakens white blood cell function, reducing the body’s ability to fight bacteria.
- Diabetic angiopathy: Damage to small blood vessels decreases nutrient delivery and waste removal from gum tissues.
- High inflammation response: Even with minimal plaque, diabetics can experience more severe gum inflammation compared to non-diabetics.
- Result: Diabetes aggravates periodontitis, making it more common and more severe.
- Directly — By Damaging Periodontal Structure (Plaque Not Required)
In severe or uncontrolled diabetes, gum damage can occur even without bacterial infection. This happens because:
- Angiopathy reduces blood flow to bone and gum tissues.
- Organic matrix of bone breaks down faster.
- Reduced regeneration and repair capacity of bone and ligaments.
- Direct collapse of periodontal structure can occur.
While rare, this type of periodontal destruction is seen in advanced diabetes. Once the structure collapses, plaque buildup can accelerate further gum disease.
- How Gum Disease Worsens Diabetes
- Inflammation raises blood sugar: Gum infections release inflammatory molecules (cytokines) into the bloodstream, increasing insulin resistance.
- Greater difficulty controlling blood sugar: Even well-managed diabetes can worsen when gum inflammation is present.
- Higher risk of diabetes complications: Poor gum health is linked to kidney disease, cardiovascular disease, and diabetic retinopathy.
📊 Scientific Evidence Supporting the Link
- American Diabetes Association: People with diabetes are 2–3 times more likely to develop gum disease.
- Journal of Periodontology: Treating gum disease can lower HbA1c levels by up to 0.4%, improving diabetes control.
- National Institute of Dental and Craniofacial Research: Chronic gum inflammation increases the risk of diabetes-related complications.
⚠️ Risk Factors That Make the Link Worse
If you have diabetes, these factors increase gum disease risk:
- Poor blood sugar control
- Smoking
- Poor oral hygiene
- Stress
- Vitamin D deficiency
- Dry mouth (common side effect of diabetes medications)
🚨 Signs You Shouldn’t Ignore
Gum Disease Symptoms:
- Red, swollen, tender gums
- Bleeding during brushing or flossing
- Persistent bad breath
- Gum recession
- Loose teeth
Diabetes-Related Oral Symptoms:
- Dry mouth
- Burning sensation in the mouth
- Slow healing after dental treatment
- Increased oral infections (thrush, abscesses)
🏠 Preventing Gum Disease in People with Diabetes
- Control Blood Sugar
Good glycemic control reduces inflammation and helps gums resist infection.
- Maintain Excellent Oral Hygiene
- Brush twice daily with fluoride toothpaste.
- Floss daily.
- Use antimicrobial mouthwash if recommended.
- Regular Dental Checkups
- Visit every 3–4 months instead of the usual 6 months.
- Stay Hydrated
Dry mouth increases plaque buildup — drink water often.
- Avoid Tobacco
Smoking doubles the gum disease risk in diabetics.
🧪 Medical & Dental Treatments
- Scaling and Root Planing – Deep cleaning to remove plaque and tartar.
- Antibiotic Therapy – To control persistent bacterial infections.
- Periodontal Surgery – For advanced cases.
- Blood Sugar Optimization – Work with your doctor to keep HbA1c in target range.
📌 Key Takeaways
- Gum disease and diabetes feed each other in a harmful cycle.
- Diabetes increases gum disease risk both indirectly (through immunity and blood vessel changes) and directly (through bone and tissue damage without bacteria).
- Treating gum disease can improve blood sugar control.
- Preventive care is the most effective strategy for breaking the cycle.
❓ 10 FAQs Not Covered in the Article
- Can gum disease cause diabetes in healthy people?
No, but severe gum inflammation may increase the risk of developing type 2 diabetes. - Is gum disease more aggressive in type 1 or type 2 diabetes?
Both types carry risk, but poorly controlled type 2 is often linked with more severe periodontal problems. - Can children with diabetes get gum disease?
Yes, especially if blood sugar is poorly controlled. - Does insulin therapy prevent gum problems?
Indirectly, yes — by keeping blood sugar in check, it reduces gum inflammation risk. - Is dry mouth in diabetes dangerous for gums?
Yes, reduced saliva allows more bacterial growth. - Can gum disease treatment lower HbA1c levels?
Yes, studies show modest but significant reductions. - Should diabetics get more frequent dental X-rays?
Yes, to detect early bone loss. - Do sugar-free gums help diabetic oral health?
Yes, especially if they contain xylitol, which reduces bacterial growth. - Is there a special toothpaste for diabetics?
Not mandatory, but fluoride toothpaste with antibacterial properties is beneficial. - Can dental infections raise blood sugar overnight?
Yes, acute infections can cause sudden spikes in blood glucose levels.
Call to Action
Explore our Gum Care Shop for essential products that support healthy gums and lasting oral hygiene.
Bleeding Gums & Gum Disease Related Reads
Gum Disease: Everything You Need to Know
Gum Pigmentation: Harmless or a Hidden Health Warning?
Can Gum Disease Be Reversed? Realistic Expectations & Proven Timeline for Recovery
Bleeding Gums in Pregnancy – Causes, Prevention & Safe Home Care for Moms-to-Be
How Smoking Affects Your Gums – The Silent Damage You Can’t Ignore
Gum Disease in Diabetics – What You Need to Know
How Stress Affects Gum Health – The Hidden Mind-Body Connection You Can’t Ignore
How Long Does Gum Treatment Take? A Complete Step-by-Step Timeline for Healthier Gums
Gum Surgery Cost Explained: Country-wise & City-wise Comparison (USA, UK, India, China)
Deep Cleaning vs Scaling: What’s the Difference for Your Gum Health?
Best Toothpaste for Gum Health: What to Use & Why It Matters
Receding Gums Treatment at Home: Effective Remedies to Protect Your Smile Naturally
Gum Disease and Heart Health Link: How Your Oral Hygiene Impacts Your Heart