Dry Mouth
Dry mouth, medically known as xerostomia, is a common condition that occurs when there is insufficient saliva production in the mouth. While it might seem like a minor inconvenience, dry mouth can lead to a range of oral health issues and impact your overall well-being. In this comprehensive guide, we delve into the various aspects of dry mouth, its causes, potential complications, and effective remedies. Our aim is to provide you with valuable insights that will help you understand and manage this condition effectively.
This post may contain affiliate links which means we may receive a small commission (at no additional cost to you) for purchases made through links. We include products we think are useful for our readers. Learn more on our Disclaimer page.
Understanding Dry Mouth
Dry mouth is characterized by the reduced production of saliva, which plays a crucial role in maintaining oral health. Saliva is a remarkable fluid vital for oral health and digestion. It moistens the mouth, aids chewing, and jumpstarts digestion with enzymes. Beyond this, it plays a pivotal role in preventing dental issues by cleaning, neutralizing, and removing food particles trapped on teeth and gums. Its antimicrobial properties fend off oral infections while aiding in the remineralization of enamel damaged by caries, abrasion, and erosion. Additionally, saliva accelerates the healing of mouth wounds, enriched by its protein and mineral content.
Common causes of Dry Mouth
Dry mouth, medically known as xerostomia, can stem from various factors, including both local conditions within the oral cavity and systemic issues affecting the body.
Local Causes of Dry Mouth:
- Adverse Habits: Engaging in habits like tobacco smoking and excessive alcohol consumption can lead to dry mouth.
- Betel Nut Chewing: Individuals who chew betel nut may experience intermittent or continuous dry mouth. Prolonged chewing can deplete available saliva, resulting in dryness.
- Excessive Alcohol-Based Mouthwashes: Overuse of mouthwashes containing alcohol can contribute to dry mouth.
- Mouth Breathing and Snoring: Breathing through the mouth and snoring can dry out the mouth by passing air directly over its surfaces.
- Prolonged Inactivity in the Mouth: Extended periods without tongue movement or other oral activities can lead to temporary dry mouth.
- Salivary Gland Duct Obstruction: Blockages, such as salivary gland stones or calcified debris, can obstruct saliva flow and cause dryness.
- Oral Thrush (Fungal Infection): Candidiasis, a fungal infection in the mouth, can disrupt normal saliva production and lead to dry mouth.
- Radiotherapy for Head-Neck Cancer: Patients undergoing radiotherapy for head and neck cancer can experience temporary or permanent damage to salivary glands, resulting in dry mouth.
These local factors can contribute to dry mouth and its associated discomfort. Addressing these causes and maintaining proper oral hygiene can help alleviate symptoms and prevent further complications.
Systemic Causes of Dry Mouth:
Dry mouth, also known as xerostomia, can be a symptom of serious health issues that impact the entire body. Here is a simplified list of systemic causes:
- Aging: Commonly observed in older adults due to factors such as nutritional deficiencies, medications’ effects, and reduced regenerative capacity.
- Anemia: Lower levels of blood hemoglobin can contribute to dry mouth.
- Alzheimer’s Disease: Neurodegenerative conditions like Alzheimer’s may result in dry mouth.
- Autoimmune Disorders: Conditions like Sjögren’s syndrome, rheumatoid arthritis, systemic lupus erythematosus, and sarcoidosis can damage salivary glands as part of their autoimmune activity.
- Chemotherapy for Cancer: Cancer patients undergoing chemotherapy may experience reduced salivary production and thicker saliva consistency.
- Cystic Fibrosis: This genetic disorder can lead to dry mouth due to its impact on various bodily functions.
- Dehydration: Insufficient fluid intake leading to dehydration can manifest as dry mouth.
- Diabetes: Poorly controlled diabetes can cause dry mouth, possibly due to altered blood flow to salivary glands.
- Hypothyroidism: Underactive thyroid function can contribute to dry mouth symptoms.
- Hormonal Changes (Menopause): Hormonal fluctuations during menopause, particularly reduced estrogen levels, can lead to diminished saliva production, resulting in dry mouth or xerostomia.
- HIV and AIDS: These conditions can damage salivary glands, leading to dry mouth.
- Medications and Drugs: Numerous medications have dry mouth as a side effect. These include anti-histamines, anti-depressants, appetite suppressors, tranquilizers, anti-hypertensives, marijuana, and recreational drugs like methamphetamine.
- Nutritional Deficiencies: Inadequate intake of certain nutrients can also contribute to dry mouth. Vitamin deficiencies, such as vitamin B3 (niacin) and vitamin B12, can impair salivary gland function and mucous membrane health, leading to dry mouth. Additionally, deficiencies in minerals like zinc and iron might also play a role in this condition.
- Stroke: Neurological conditions like stroke might lead to disruptions in saliva production.
- Stress, Anxiety, and Depression: Mental health factors can influence salivary function and contribute to dry mouth.
These systemic factors can contribute to the development of dry mouth. Recognizing the underlying causes is crucial for effective management and symptom relief.
Recognizing Signs and Symptoms of Dry Mouth
Dry mouth, or xerostomia, manifests through various indicators, including:
- Difficulty in Chewing and Swallowing: Saliva assists in breaking down food, making it easier to chew, swallow and digest. Insufficient saliva makes chewing, swallowing and digestion less efficient, potentially leading to nutritional deficiencies.
- Speech Challenges: Reduced saliva affects speech clarity, causing speech impediments and a hoarse voice.
- Persistent Bad Breath: Dry mouth hampers the removal of food particles and bacteria, often resulting in ongoing bad breath.
- Increased Risk of Tooth Diseases: Saliva acts as a natural defense against tooth diseases by neutralizing acids and providing minerals to strengthen enamel. A lack of saliva can lead to an increased risk of cavities and gum problems.
- Persistent Thirst: Frequent thirst despite adequate fluid intake might point to dry mouth.
- Dry or Sticky Sensation: A dry or sticky feeling in the mouth, throat, or tongue can signal reduced saliva.
- Difficulty in Speaking or Swallowing: Impaired speech enunciation and swallowing discomfort are common dry mouth symptoms.
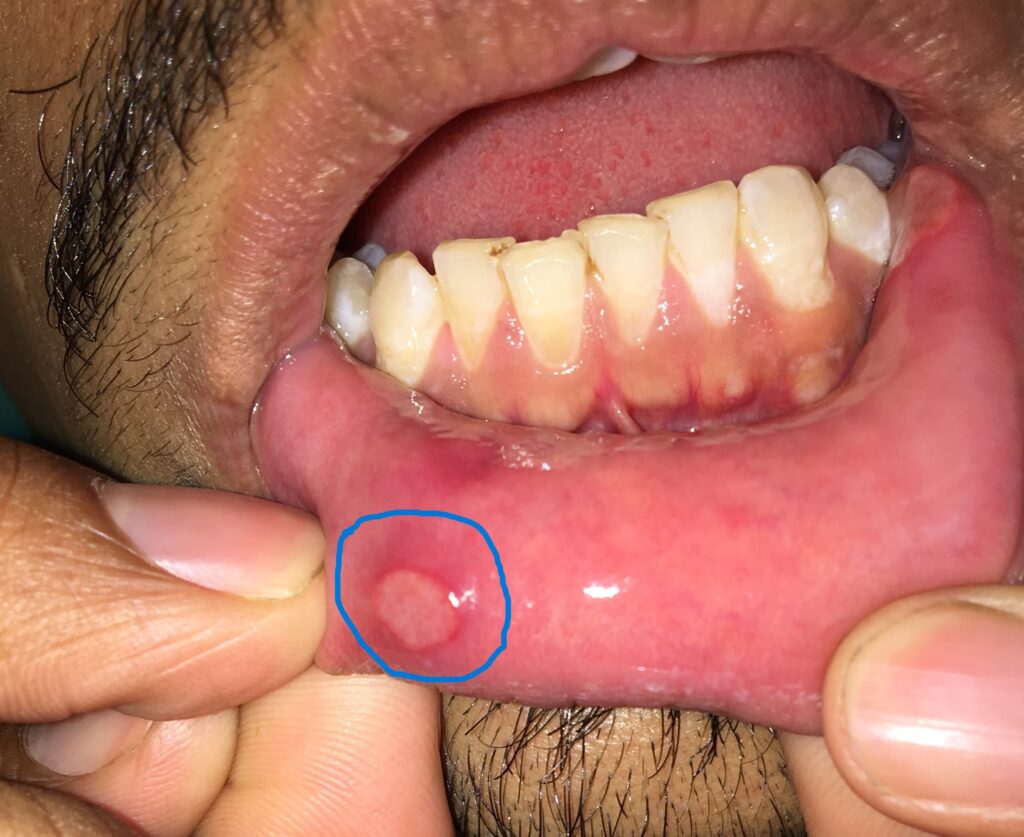
- Oral Irritation: Dryness may lead to mouth sores, ulcers, and cracked lips.
- Altered Taste: Changes in taste perception or experiencing a metallic taste could indicate dry mouth.
Should you notice these signs or symptoms persistently, seeking consultation is advisable. A dentist can provide guidance and recommend appropriate measures to address dry mouth and its associated effects.
Impact of Dry Mouth on Oral and Systemic Health
Oral Complications:
- Tooth Decay: Reduced saliva leaves teeth vulnerable to decay as it can’t neutralize acids or remineralize enamel effectively. This leads to cavities.
- Gum Disease: Lack of saliva allows harmful bacteria to flourish, contributing to gingivitis and periodontitis, which can lead to tooth loss.
- Bad Breath: Insufficient saliva fails to wash away food particles and bacteria, resulting in persistent bad breath.
- Mouth Infections: Dryness creates an environment where infections, like thrush, can thrive.
- Mouth Sores: Dry oral tissues are more prone to irritation, leading to the development of mouth sores and ulcers.
- Difficulty in Wearing Dentures: Dry mouth makes wearing dentures uncomfortable due to reduced lubrication and increased friction.
- Tonsillar stones: Dry mouth can contribute to the formation of tonsillar stones, leading to bad breath, throat irritation, and infection risk.
Systemic Complications:
- Digestive Problems: Reduced saliva affects the initial digestion of food, impacting nutrient absorption and overall digestive health.
- Malnutrition: Difficulty in chewing and swallowing can lead to a lack of essential nutrients, causing malnutrition over time.
- Speech Difficulties: Insufficient saliva affects tongue and mouth movements, leading to speech impediments.
- Increased Infections: Saliva’s antimicrobial properties help combat infections. Dry mouth can elevate the risk of oral and throat infections.
- Diabetes Management: Diabetes is one of the causes of dry mouth. Dry mouth complicates diabetes care, as saliva helps regulate blood sugar levels by initiating digestion of carbohydrates.
- Respiratory Issues: Saliva plays a role in clearing airway irritants. Dry mouth might lead to respiratory discomfort.
- Heart Health: Emerging research suggests a link between chronic dry mouth and cardiovascular health, though more studies are needed.
- Joint Pain: Some systemic conditions that cause dry mouth, like Sjögren’s syndrome, can also lead to joint pain.
- Quality of Life: Both orally and systemically, dry mouth can diminish quality of life by causing discomfort, impacting social interactions, and affecting overall well-being.
Addressing dry mouth promptly is essential to prevent these complications and maintain optimal oral and systemic health. Consulting a healthcare professional can help identify underlying causes and develop effective management strategies.
Prevention, Remedies, and Care for Dry Mouth
- “Consult a specialist or oral physician as soon as you realize you are suffering from dry mouth. This proactive step can help prevent the worsening of the condition and address any underlying serious health issues, instead of relying solely on self-remedies.”
- Avoid Triggers: Steer clear of factors that contribute to dry mouth, such as tobacco, alcohol, and betel-nut chewing.
- Balance Diet: Maintaining a well-balanced diet rich in essential vitamins and minerals are crucial for preventing these nutritional-related causes of dry mouth. Avoid or limit caffeine, sugary, acidic, spicy, and dry foods, as well as excessively hot or cold drinks. If you suspect nutritional deficiencies as a potential factor, consulting a healthcare professional can help address and manage the issue effectively.
- Oral Hygiene: Maintain regular oral care routines, including brushing, flossing, and using a water jet device.
- Dental Check-ups: Schedule periodic dental visits to monitor your oral health and address any emerging issues.
- Hydration: Stay hydrated by frequently sipping water or sugar-free fluids. Sipping water while eating aids in swallowing.
- Salivary Substitutes: Over-the-counter salivary substitutes, toothpaste, and rinses can offer relief.
- Stimulate Saliva: Opt for foods that stimulate salivary production like sugarless candies or vitamin ‘C’ containing foods. Sugar-Free Gum or candy containing xylitol can stimulate saliva production.
- Fluoride Use: Opt for fluoride toothpaste and rinses, consulting your dentist for therapeutic fluoride applications.
- Medication Review: Consult your doctor to adjust medications contributing to dry mouth. Astringents: Avoid substances with astringent properties.
- Nasal Breathing: Try to breathe through your nose rather than your mouth to reduce dryness, consulting ENT specialists if needed.
- Hydration and Humidifier: Use a humidifier in your room to combat dryness. Ensure consultation if you have respiratory issues.
Taking proactive steps and adhering to these practices can help manage dry mouth symptoms and enhance your overall oral comfort.
Dry mouth saliva substitute: https://amzn.to/3sjOk1L
Dry mouth moisturizing gum: https://amzn.to/3KKc7hX
Sugar-free chewing gum: https://amzn.to/3QKJzZh
Manual extra soft toothbrushes for adults: https://amzn.to/3YHu5aG
Manual extra soft toothbrushes for kids: https://amzn.to/47DH0ym
Electric toothbrush for adults: https://amzn.to/3P7v68P
Electric toothbrush for kids: https://amzn.to/44lZsZB
Fluoride toothpaste: https://amzn.to/3ODvQ44
Fluoride toothpaste for kids: https://amzn.to/3QLDJqA
Water flossers: https://amzn.to/45zdiJ6
Cordless water floss: https://amzn.to/3KLiNwk
Dental floss: https://amzn.to/3QIQyC4
Dental floss with holder and replaceable head: https://amzn.to/3qtQVpD
Antiseptic mouthwash (Alcohol-free): https://amzn.to/47AoRBo
Treatment and Management of Dry Mouth
Effective management of dry mouth involves:
- Identifying and Addressing Underlying Causes: Pinpointing and mitigating the root cause of dry mouth is essential. Work closely with your healthcare provider to determine and treat the cause.
- Symptomatic Relief: Focus on alleviating discomfort and preventing complications associated with dry mouth. This includes replenishing lost salivary secretions and addressing issues like difficulty in eating, dental decay, oral infections, and burning mouth sensation.
- Stimulating Salivary Glands: Therapies and medications that promote the regeneration or repair of salivary glands can be beneficial.
- Personal Insights: Share comprehensive and accurate information about your condition with your healthcare provider. Your insights into your own experiences can aid in identifying the cause and tailoring treatment.
- Oral Health Maintenance: Consistent oral hygiene measures are crucial due to the significant impact of chronic dry mouth on oral health. Emphasize preventive measures, including plaque and calculus removal (scaling), treating dental decay, gum diseases, fungal or other oral infections, and fluoride treatments. Regular dental check-ups are vital.
- Medication Adjustment: If a specific medication is causing dry mouth, consult your doctor before making any changes. They may adjust the dosage or switch to a different drug with lower chances of causing dry mouth.
- Investigations: Your doctor may recommend tests to rule out both local and systemic conditions contributing to dry mouth.
- Saliva-Stimulating Medications: In some cases, your healthcare provider might prescribe medications that stimulate saliva production.
Saliva Stimulating Therapies
saliva-stimulating therapies available to help alleviate dry mouth. These therapies aim to enhance salivary gland function and increase saliva production. Some methods include:
- Salivary Gland Massage: Gently massaging the salivary glands can stimulate saliva flow. This manual technique can be performed under the guidance of a healthcare professional to prevent unintended effects.
- Saliva-Stimulating Medications: Certain medications can promote saliva production. These medications, prescribed by healthcare providers, help address dry mouth by stimulating the salivary glands.
- Electrical Stimulation: Some advanced treatments involve electrically stimulating the salivary glands through techniques like electroacupuncture or transcutaneous electrical nerve stimulation (TENS). These methods can encourage salivary secretion.
- Nerve Stimulation: Nerve stimulation therapies, like using small electrical currents or biofeedback techniques, can activate neural pathways associated with salivary gland function, potentially increasing saliva production.
- Xylitol Containing Products: Chewing gum or lozenges containing xylitol can stimulate saliva production, providing temporary relief from dry mouth symptoms.
- Acupuncture: Some individuals find relief from dry mouth through acupuncture, a traditional practice that involves inserting thin needles into specific points on the body.
It’s important to consult with healthcare professionals, including oral physicians or neurologists, to determine the most suitable saliva-stimulating therapy based on your individual needs and medical history.
Salivary Gland Massage
Your doctor may suggest salivary gland massage to encourage saliva production or gland regeneration/repair. This technique can be helpful but requires proper guidance to prevent unintended outcomes.
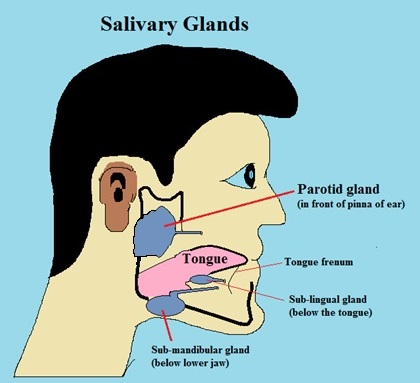
Normal location of salivary glands will help you in massaging them.
- Parotid Gland Massage: Stimulate parotid glands by gently rotating your fingers in front of each ear and sliding them forward towards the opening inside your mouth.
- Submandibular Gland Massage: Massage under your lower jaw using gentle rotations and slides towards your chin.
- Sublingual Gland Massage: Place your thumb beneath your lower jaw, behind the chin, and massage similarly to the submandibular gland technique.
- Frequency: Perform these massages 2-3 times a day for 1-2 minutes each time, ensuring consistent but gentle pressure.
Note: Consult your healthcare provider or oral physician before attempting salivary gland massage, as proper technique and timing are essential to avoid potential complications.
By adhering to these treatment and management strategies, you can effectively alleviate dry mouth symptoms and enhance your overall comfort.
Conclusion
Dry mouth, medically referred to as xerostomia, stems from insufficient salivary production by the glands within the oral cavity. While it primarily affects oral comfort, it also holds a significant role in maintaining overall bodily health and functions. Understanding the causes and adopting appropriate care measures are essential for managing this condition effectively.
Dry mouth can be either a transient occurrence or a persistent concern, with its significance extending beyond mere discomfort. It serves as a potential indicator of serious systemic conditions, including Sjögren’s syndrome, rheumatoid arthritis, systemic lupus erythematosus, sarcoidosis, Parkinson’s disease, and diabetes. This underscores the importance of recognizing dry mouth as a valuable diagnostic sign for underlying health issues.
Medications, often integral to managing various ailments, can paradoxically lead to dry mouth as a common side effect. Adjusting medication dosages or considering alternative drugs under professional guidance can help mitigate this concern. It’s crucial to avoid self-modification and consult medical professionals for optimal outcomes.
The impact of chronic dry mouth on oral health cannot be overstated. Consistent oral hygiene practices and preventive measures are paramount to prevent complications like dental decay, gum diseases, and oral infections. While certain treatments offer symptomatic relief, addressing the underlying cause requires a comprehensive approach. Collaboration with oral physicians is essential to determine the root cause and tailor appropriate interventions.
In summation, dry mouth transcends a mere inconvenience, offering insights into both oral and systemic well-being. Its management demands a multidimensional approach, spanning from understanding causative factors to adopting proactive oral care and seeking professional guidance. By integrating these measures, individuals can navigate the challenges of dry mouth with improved comfort, oral health, and overall quality of life.
FAQs about Dry Mouth
Q: Can stress contribute to dry mouth?
Stress can indeed lead to dry mouth. When you’re stressed, your body’s fight-or-flight response can reduce saliva production.
Q: Are there any natural remedies for dry mouth?
Yes, there are. Drinking water, chewing sugar-free gum, and consuming foods rich in water content, like watermelon and cucumber, can help alleviate dry mouth.
Q: Can certain foods worsen dry mouth?
Absolutely. Foods high in salt or spice can intensify dry mouth symptoms. Avoiding or reducing their consumption can be beneficial.
Q: Is dry mouth a common side effect of aging?
Yes, dry mouth is more prevalent in older adults. However, it’s important to note that it’s not a normal part of aging and should be managed.
Q: How does smoking affect dry mouth?
Smoking can exacerbate dry mouth. It reduces saliva production and contributes to overall oral health problems.
Q: When should I see a doctor for my dry mouth?
If your dry mouth persists for an extended period, it’s advisable to consult a healthcare professional. They can help identify the underlying cause and recommend appropriate treatments.