Gum Disease
Gum disease, also known as pyorrhea, is a common dental problem that affects millions of people worldwide. In fact, studies have shown that more than 80% of individuals over the age of 35 are affected by this condition. It’s important to note that gum disease can even begin in teenage years. That’s why, it’s crucial to take steps to maintain good oral health from a young age to reduce the risk of developing gum disease later in life. It starts with bacterial inflammation of the gums and can progress to serious complications, including tooth loss and general health issues. Gum disease is preventable and early detection is key to successful treatment. In this article, we will discuss everything about gum disease, including causes, risk factors, symptoms, and how it starts and progresses, treatment options and most importantly, how to prevent it.
Gingivitis and periodontitis are usually asymptomatic in most people, which poses a major problem especially in individuals who are irregular in dental visits and do not inspect their own oral health may be diagnosed with severe periodontitis that can be irreversible and sometimes even untreatable. Furthermore, symptoms in the early stages of periodontitis may not be easily noticeable. Your dentist will probably be the first to identify them. Therefore, it is crucial to know everything about gum disease.
What is Gum Disease?
Gum disease, also known as periodontal disease or pyorrhea, is an inflammatory destruction of the supporting tissues of the teeth. It is caused by the accumulation of plaque on your teeth that hardens into tarter unless removed constantly. Plaque is a sticky film of bacteria that forms on your teeth and gums after eating. When plaque is not removed by brushing and flossing, it causes infection, inflammation, and destruction of the gums and bone that supports your teeth.
How Gum Disease Start and Progresses?
Causes
The main cause of gum disease and tooth decay is the bacteria present in the dental plaque. If plaque is not removed by proper brushing and flossing, it can harden into tarter, which creates favorable environment for more plaque to accumulate. This leads to a cycle of plaque and tarter build-up that can cause gum disease. Gum disease typically occurs when tarter builds up under your gums and between teeth. Most importantly, tarter build-up is symptomless (silent) and cannot removed by brushing or flossing, leading to undetected progression of gum disease.
Risk Factors
Risk factors are not the actual cause of gum disease but can make an individual more susceptible to developing the disease or making it more serious.
Local Factors:
- Poor oral hygiene – Poor oral hygiene leads to plaque and tarter build-up, which increases bacterial load and causes gum inflammation and destruction.
- Irregular dental visits – Irregular dental visits can lead to the initial stages of gum disease going unnoticed, allowing it to progress and become more difficult to treat. One more important point that tarter build-up is often asymptomatic and can go unnoticed under gums and between teeth, and it cannot be removed by brushing and flossing alone and only professionals can detect and remove it.
- Misaligned or crowded teeth – It is difficult to clean misaligned or crowded teeth, which leads to build-up of plaque and tarter. Misaligned teeth usually subjected to irregular chewing forces that further weaken their supporting structure, making them susceptible to gum disease even with minimal plaque and tarter build-up.
- Trauma to teeth or gums – Trauma from occlusion refers to damage caused by improper alignment of teeth. Misaligned teeth or crooked bite usually subjected to irregular chewing forces that damages and weaken their supporting structure, making them susceptible to gum disease even with minimal plaque and tarter build-up.
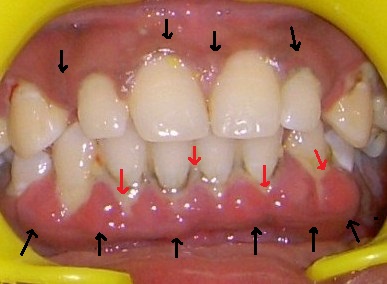
- High attachments of frenum – High oral frenum pull the gums away from the teeth during oral activities, creating pockets between teeth and gums where plaque and tarter can accumulate that leads to gum disease.
High frenum pulls the gums down
- Habit of teeth clenching or grinding – Habit of clenching or bruxism puts excessive pressure on the teeth and gums, leading to gum recession and making them susceptible to gum disease even with minimal plaque and tarter build-up.
High oral frenum, teeth clenching or grinding, and the trauma from a crooked bite can cause gum disease even with little plaque and tarter build-up, and can occur earlier than gum disease caused only by plaque and tarter accumulation.
- Rough or faulty dental restoration or appliance – A rough or faulty dental restoration provides a favorable surface that is difficult to clean, allowing more accumulation of plaque and tarter, which can cause gum disease.
- Chewing tobacco or smoking – Chewing tobacco or smoking reduces blood flow to the gums, weakens immune system, and promote accumulation of tarter build-up and the growth of harmful bacteria. Tobacco also damages gums and delays wound healing.
- Mouth breathing – Mouth breathing can cause gum disease by reducing saliva flow, drying out the mouth and gums, which reduces cleansing action and favors tarter formation. Dry mouth also increases the growth of harmful bacteria and increases the risk of infection and inflammation, leading to gum disease.
Systemic Factors:
- Diabetes – Diabetes weakens body’s immunity to fight off infections and inflammations.
- Hormonal Imbalances – Hormonal imbalances increases inflammation and reduces the body’s ability to fight off infections in the gums.
- Pregnancy – Pregnancy can lead to development of new gum disease or aggravate the existing gum disease due to hormonal changes and immune system alterations.
- Genetic Predisposition – Genetic changes can make the gums more susceptible to infection or inflammation in response to other risk factors, such as poor oral hygiene or smoking.
- Stress – Stress can cause hormonal imbalance and weaken our immune system, leading to increased risk of gum inflammation.
- Medications that cause dry mouth – Certain medications such as antidepressants and blood pressure medications, can reduce saliva flow, leading to increased risk of gum disease due to reduced cleansing and decreased protection against harmful bacteria.
- Osteoporosis – Osteoporosis can weaken the jawbones, making it easier for bacteria to penetrate and cause gum disease.
- Respiratory disease – respiratory disease and gum disease can exacerbate each other, as the microbes in the mouth can worsen respiratory problems, and respiratory disease can increase the risk of gum disease by increasing inflammation and weakening the immune system.
- Blood cancer – Blood cancer can weaken the immunity, make the gums more vulnerable to infection. Cancer cells can invade gum tissues, which can result in “boggy” gum enlargement that may cause the gums to bleed.
- Vitamin C deficiency – Vitamin C plays an important role in regeneration and repair of collagen in the gums, bones and connective tissues of the body, that’s why it’s deficiency can lead to spongy and bleeding gums.
Though both local and systemic factors can contribute to gum disease, local factors mainly poor oral hygiene plays a major role in its development. However, maintaining good oral hygiene practices, such as brushing and flossing regularly, and regular professional cleaning can significantly reduce the chances of developing gum disease.
Stages of Gum Disease
There are two main stages of gum disease: Early and Advanced stage
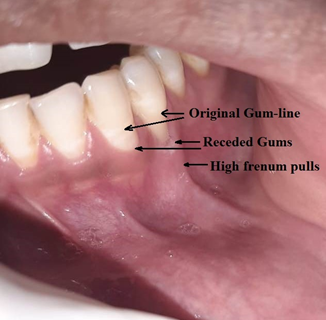
- Gingivitis – This is an early stage.
- Periodontitis – This is an advanced stage.
Gingivitis: This is the early stage of gum disease that affects only the collar of the gums around your teeth. Gingivitis is an initial stage of periodontitis. It is caused by bacteria in the plaque. But if left undetected and untreated, gingivitis can progress to periodontitis. Reversing gingivitis in its initial stage is important to prevent it from progressing to more advanced stages of gum disease, periodontitis.
Gingivitis: An early gum disease
Periodontitis: Periodontitis is commonly known as pyorrhea. It is caused by bacteria in the plaque. If left untreated, gingivitis can progress to periodontitis, which causes inflammation to spread deeper into the gums and lead to the destruction of soft tissues and bone that supports your teeth. If left undetected and untreated, periodontitis can lead to tooth loss and other health problems.
Stages of Periodontitis
There are several stages of periodontitis, ranging from mild to severe, based on severity of the disease and the damage to supporting gums and bone. Here are the stages of periodontitis:
- Gingivitis: This is the first stage of periodontitis.
- Early Periodontitis: During this stage, the damage begins to spread below the gum line, and the supporting bone starts to deteriorate. Sign and symptoms of early periodontitis include red, swollen, and bleeding gums, bad breath similar to gingivitis, and there may also be mild gum recession.
- Moderate Periodontitis: At this stage, the bone loss becomes more significant, and the teeth may become loose, or even start to shift or move around. The gums may recede more, exposing more of tooth’s root. There may be pus discharge from the gums.

Mild to moderate periodontitis
4. Advanced Periodontitis: In the final stage, the bone and gum tissues are severely damaged, and the teeth may become very loose or even fall out. There may be severe gum recession and noticeable changes in bite and alignment of teeth. You may experience pain or discomfort in the affected region.
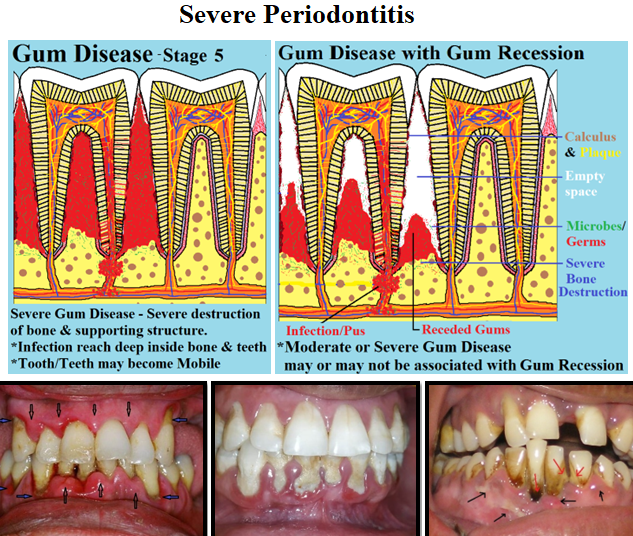
Severe periodontitis
Sign and symptoms of Gum Disease
Gingivitis
- Red and swollen gums.
- Gums that bleed easily when you brush or floss your teeth.
- Bad breath.
- Rarely, gums can become tender and sore to touch.
Periodontitis
Periodontitis can have same features as gingivitis, but it also presents additional features like:
- Pocket formation – Pocket or gap may form between teeth and gums, which can trap more and more food and bacteria.
- Tarter and plaque build-up cycle – Pocket provide more space for tarter and plaque build-up.
- Gum recession – Gums may recede or pull away from the teeth, exposing more of the tooth’s surface.
- Sensitivity – Periodontitis can cause sensitivity in teeth and gums due to destruction of gum and bone tissues, and causing gum recession, which exposes nerve endings.
- Bone loss – Bone loss around your teeth, which can be visible on x-rays.
- Teeth mobility – You may feel mobility in your teeth, where your teeth are loose or shifting, that can lead to gaps between teeth.
- Disturbed teeth–bite – Changes in the way your teeth fit together when biting or chewing.
- Inability to chew – Severe periodontitis can lead to an inability to chew properly.
- Pus – formation of pus in the pocket between your teeth and gums.
- Pain – Similar to gingivitis, periodontitis rarely causes pain.
- Discomfort – Discomfort on chewing can occur in advanced stages of periodontitis, when teeth are mobile.
In summary, gingivitis is inflammation and destruction of gums, whereas periodontitis is inflammation and destruction of both the gums and supporting bone.
Treatment of Gum Disease
Gingivitis and Mild Periodontitis
The treatment of gingivitis and mild periodontitis typically involves:
- Professional dental cleaning (scaling and root planing) to remove plaque and tarter.
- Treatment for other risk factors, such as trauma from a crooked bite, high oral frenum, and teeth-crowding.
- Good oral hygiene practices such as regular brushing and flossing at home.
- Lifestyle changes, such as quitting smoking and improving diet.
- Consult medical physician to rule out systemic diseases that aggravate gum disease.
- Regular dental check-up and cleanings are important to maintain good oral health and to prevent further damage.
Moderate Periodontitis
The treatment of moderate periodontitis includes all the treatments mentioned for gingivitis and mild periodontitis, such as scaling and root planning and good oral hygiene practices at home. In addition, moderate periodontitis may require deep cleaning and surgical intervention to remove damaged tissues, correct defects and rehabilitation with soft-tissue and bone grafting, the use of antibiotics, and addressing any other precipitating factors that may have contributed to the disease. Regular dental check-up and maintenance are also essential for controlling the disease and preventing further damage. Your dentist or periodontist may design a personalized treatment plan for effective management of moderate periodontitis.
Severe Periodontitis
The treatment of severe periodontitis includes all the treatments mentioned for moderate periodontitis, such as deep cleaning and surgical interventions such as correcting defect, tissue grafting and regeneration procedures. However, severe periodontitis requires more intensive self-care and frequent professional treatments than moderate periodontitis.
In some cases of severe periodontitis, where teeth cannot be saved, extraction may be necessary. After extraction, the missing teeth can be replaced with artificial teeth such as removable or fixed prostheses or dental implants.
How can Gum Disease be Prevented?
Proper and consistent oral hygiene care can prevent gum disease. This includes:
- Maintain good oral hygiene habits, including brushing twice a day with fluoride toothpaste, and flossing daily.
- Daily clean your tongue using a tongue brush or scrapper.
- Regularly visit your dentist or periodontist for check-ups and cleanings to catch any potential issues early on.
- Eat healthy diet that is low in sugar and high in vitamins and nutrients.
- Chew your food properly.
- Drink adequate amount of water daily.
- Address local factors, such as trauma from crooked bite, crowded teeth, and high frenums, that can exacerbate gum disease by getting timely treatment.
- Avoid tobacco products as they can increase the risk of gum disease.
- Treat any underlying medical conditions, such as diabetes, that may increase the risk of gum disease.
- Performing periodic self-examination is also important to catch any potential issues with gum disease early on.
By following these steps, you can help prevent and manage gum disease, and protect your oral and overall health.
Conclusion
Gum disease is a very common that can cause tooth loss and other serious general health problems. One of the major challenges with this disease is that it is often asymptomatic (silent), making it difficult to detect until it has already caused significant damage. Many people also mistakenly believe that regular oral hygiene practices, such as brushing and flossing are enough to prevent gum disease, but the reality is that these practices may not effectively clean hard-to-reach areas of the teeth and gums.
To prevent and manage gum disease, it is crucial to prioritize prevention, early detection and treatment. This means understanding gum disease, as well as taking steps to maintain good oral hygiene, and regularly visiting a dentist or periodontist for check-ups and cleanings. With the proper care and attention, you can keep your gums healthy, and maintain a beautiful, confident smile and protect your oral as well as overall health. All you need is to start early and practice consistently.
FAQs
- Can gum disease be reversed?
Yes, initial stages of gum disease, such as gingivitis, even mild to moderate periodontitis can be reversed with proper treatment and good oral hygiene habits.
- How can I detect if I have gum disease?
Common sign and symptoms of gum disease include bleeding gums, red and swollen gums, receding gums, bad breath and loose teeth.
- How can I prevent gum disease?
You can prevent gum disease by following good oral hygiene practices, eating a balanced diet, avoiding tobacco use, addressing local as well as systemic risk factors, and visiting your dentist regularly for check-ups and cleanings to catch any potential issues early on.
- Can gum disease cause tooth loss?
Yes, if left undetected and untreated, early gum disease can progress to more advanced stages, causing damage to the supporting tissues of the tooth, and ultimately leading to tooth loss.
- Can gum disease cause systemic health issues?
Gum disease can cause systemic health issues by allowing bacteria from the mouth to enter the bloodstream and potentially affect other parts of the body.
- Are certain people more susceptible to gum disease than other?
Yes, genetics play a role in the development of gum disease, and certain health conditions, such as diabetes, can increases the risk of gum disease. However, maintaining good oral hygiene practices and regular dental visits can significantly reduce the risk of gum disease.
- Can I use mouthwash to prevent gum disease?
It is recommended to avoid using anti-germ mouthwashes on a daily basis, unless advised by your doctor. These mouthwashes should only be used in specific situations and for specific period, such as during acute infections, hospitalization, or postoperative phase. Mouthwashes can also lead to regular exposure to chemicals, including antibiotics. However, it is acceptable to occasionally use a small amount to freshen your breath and combat bad odor. Mechanical measures like toothbrushing and flossing have been proven to be more effective in keeping teeth free from plaque than chemical measures like mouthwashes and antibiotics. Remember, mouthwash should not be used as a substitute for proper hygiene practices such as brushing and flossing.