Leukoplakia is one of the most common oral precancerous lesion, characterized by persistent white patches in the mouth. Recognizing and addressing leukoplakia early can significantly reduce the risk of progression to oral cancer. In this comprehensive guide, we delve into the features, types, causes, prevention strategies, self-screening techniques, and treatment options for leukoplakia.
What Is Leukoplakia?
Leukoplakia refers to a white patch or plaque that develops in the oral cavity and cannot be wiped away. It is often considered an oral potentially malignant disorder (oral precancer), with some cases showing a predisposition to progress into oral cancer. While not all leukoplakia cases are malignant, early diagnosis is critical.
Features of Leukoplakia
Leukoplakia presents distinct clinical features that make it identifiable:
- White Patches: Persistent, thickened, and often slightly raised white areas in the mouth.
- Irregular Borders: Edges of the patches may be well-defined or blended into surrounding tissues.
- Asymptomatic Nature: Typically painless in its early stages, but some individuals may experience mild irritation.
- Non-Removable Patches: The white lesions cannot be scraped off, distinguishing leukoplakia from other conditions like candidiasis.
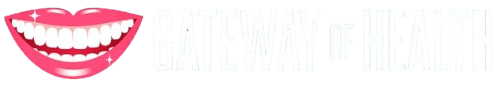
Homogenous leukoplakia
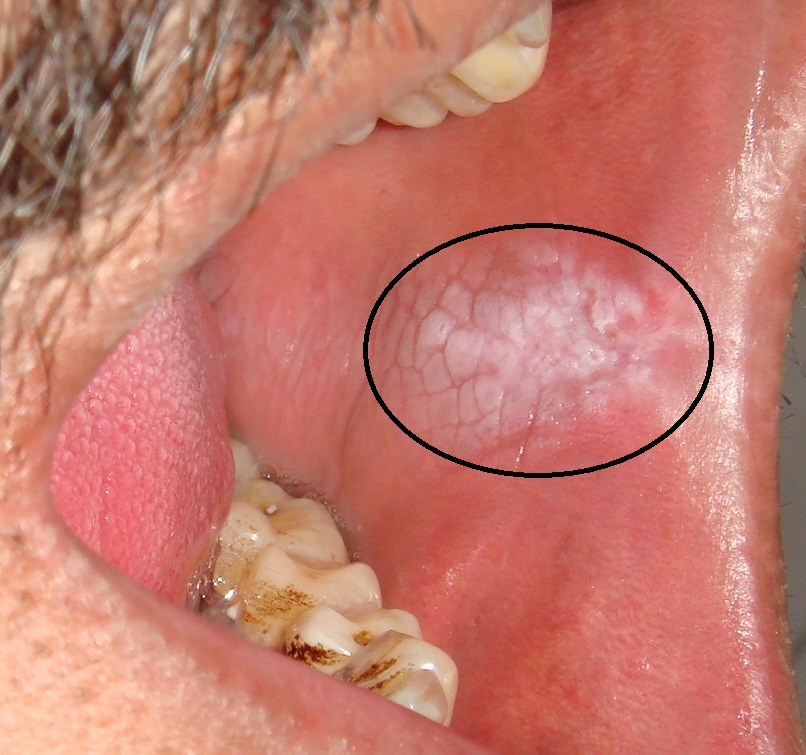
Non-homogenous leukoplakia
Types of Leukoplakia
Leukoplakia is broadly classified into two types based on appearance:
- Homogeneous Leukoplakia
- Appearance: Uniform, flat, thin white patches with a smooth surface.
- Risk: Lower potential for malignant transformation compared to non-homogeneous leukoplakia.
- Non-Homogeneous Leukoplakia
- Appearance: Irregular white patches with red areas (erythroleukoplakia), nodular or verrucous textures.
- Risk: Higher potential for malignancy due to its irregular nature.
Causes of Leukoplakia
Leukoplakia is associated with several risk factors that contribute to its development:
- Tobacco Use: Smoking or chewing tobacco is the most common cause.
- Alcohol Consumption: Chronic alcohol use increases the risk.
- Chronic Irritation: Poorly fitting dentures, rough teeth, or repetitive trauma to the oral tissues.
- Areca Nut Chewing: Particularly common in some cultural practices.
- Immunosuppression: Reduced immunity may predispose individuals to leukoplakia.
- Human Papillomavirus (HPV): Some studies suggest a link between leukoplakia and high-risk HPV strains.
How to Prevent Leukoplakia
Preventing leukoplakia involves reducing exposure to known risk factors and adopting healthy oral habits:
- Quit Tobacco: Eliminate smoking and smokeless tobacco products.
- Limit Alcohol: Reduce or avoid excessive alcohol consumption.
- Maintain Oral Hygiene: Brush and floss regularly to reduce irritation and infection.
- Address Chronic Irritation: Repair or replace ill-fitting dental appliances and smooth sharp teeth.
- Eat a Balanced Diet: Consume foods rich in antioxidants, such as fruits and vegetables, to support oral health.
- Regular Dental Check-Ups: Early detection during routine visits can help identify and manage leukoplakia promptly.
Self-Screening for Leukoplakia
Self-examination can be a valuable tool for early detection. Here’s how you can perform a self-screening:
- Check Your Mouth Regularly: Use a mirror to examine your gums, tongue, cheeks, and the roof of your mouth for white patches.
- Look for Non-Removable Lesions: Ensure the white patches cannot be scraped off.
- Pay Attention to Red Areas: Red spots combined with white patches (erythroleukoplakia) may signify higher risk.
- Note Any Changes: Monitor the size, texture, and thickness of the patches over time.
- Consult a Dentist: If you notice persistent patches lasting more than two weeks, seek professional advice.
Treatment Options for Leukoplakia
Treatment for leukoplakia focuses on eliminating the underlying cause and managing the lesion to reduce the risk of malignancy:
- Lifestyle Changes
- Quit Risky Habits: Stop smoking, tobacco use, and alcohol consumption.
- Improve Diet: Incorporate more fruits, vegetables, and essential nutrients.
- Medical Interventions
- Topical Medications: Retinoids or corticosteroids may be applied to reduce the size of the lesion.
- Antifungal Treatment: In cases of superimposed infections like candidiasis.
- Surgical Options
- Excision: Complete removal of the lesion via scalpel or laser surgery.
- Cryotherapy: Freezing the lesion to destroy abnormal cells.
- Regular Monitoring
- Follow-Up Visits: Frequent evaluations to monitor changes in the lesion.
- Biopsy: Necessary for lesions showing signs of high-risk features like induration, ulceration, or rapid growth.
Conclusion
Leukoplakia is a significant oral health concern that requires attention due to its potential for malignant transformation. Early recognition, lifestyle changes, and appropriate treatment can dramatically reduce the risk of progression to oral cancer. Regular dental check-ups and self-screening play a pivotal role in early detection and management.
Q&A: Common Questions About Leukoplakia
Q: Is leukoplakia always cancerous?
A: No, most cases of leukoplakia are benign, but some may progress to oral cancer. Regular monitoring is essential.
Q: How long does it take for leukoplakia to turn into cancer?
A: The transformation depends on factors like lesion type, size, and risk factors. Non-homogeneous leukoplakia poses a higher risk.
Q: Can leukoplakia heal on its own?
A: Mild cases may regress after eliminating risk factors like tobacco and alcohol. However, professional evaluation is recommended.
Q: Is leukoplakia painful?
A: Most leukoplakia lesions are painless, but irritation or discomfort may occur in some cases.
Q: How can I differentiate leukoplakia from other white patches in the mouth?
A: Leukoplakia cannot be scraped off, unlike conditions such as oral thrush. A dental professional can confirm the diagnosis.
By understanding and addressing leukoplakia early, you can take proactive steps to protect your oral health and overall well-being. Regular monitoring and professional care are key to managing this condition effectively.