Introduction
The Intersection of Rare Medical Conditions and Dental Emergencies
Rare medical conditions often present unique challenges in dental care. In some cases, dental professionals may be the first to identify signs of these conditions during routine examinations. For instance, certain connective tissue disorders can manifest through oral symptoms, leading patients to seek emergency dental care. These conditions can significantly influence dental treatment protocols, necessitating modifications to standard procedures. Both patients and dentists must be aware of these potential issues to ensure safe and effective care.
Understanding Ehlers-Danlos Syndrome (EDS) and Its Oral Health Implications
In this article, we will explore Ehlers-Danlos Syndrome (EDS), a group of connective tissue disorders. We will delve into its causes, symptoms, and distinctive features, with a particular focus on oral manifestations. Additionally, we will discuss diagnostic approaches, preventive measures, and general care strategies. Emphasis will be placed on the specific oral care modifications required for individuals with EDS, including patient instructions and the pivotal role of dental professionals in managing this condition.
What is Ehlers-Danlos Syndrome?
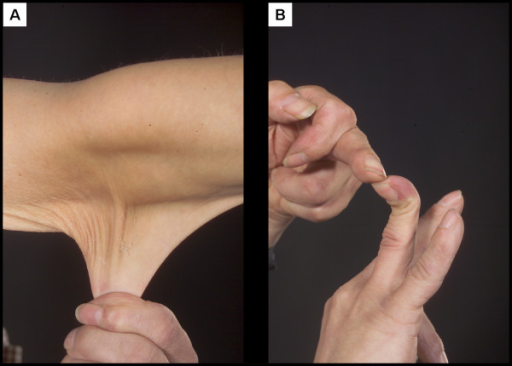
Ehlers-Danlos Syndrome (EDS) encompasses a group of genetic disorders affecting connective tissues, primarily the skin, joints, and blood vessel walls. These disorders are characterized by varying degrees of joint hypermobility, skin hyperextensibility, and tissue fragility. The severity and specific symptoms can differ based on the EDS subtype.
Causes of Ehlers-Danlos Syndrome
EDS is typically caused by genetic mutations that affect collagen production or structure, leading to weakened connective tissues. These mutations can be inherited in an autosomal dominant or recessive pattern, depending on the specific EDS type.
Symptoms and Features of Ehlers-Danlos Syndrome
Common symptoms of EDS include:
- Joint Hypermobility: Unusually flexible joints that extend beyond the normal range.
- Skin Hyperextensibility: Skin that can be stretched further than usual.
- Tissue Fragility: A tendency for the skin to bruise, tear, or scar easily.
Other features may involve cardiovascular complications, chronic pain, and, notably, oral manifestations.
Oral Manifestations of Ehlers-Danlos Syndrome
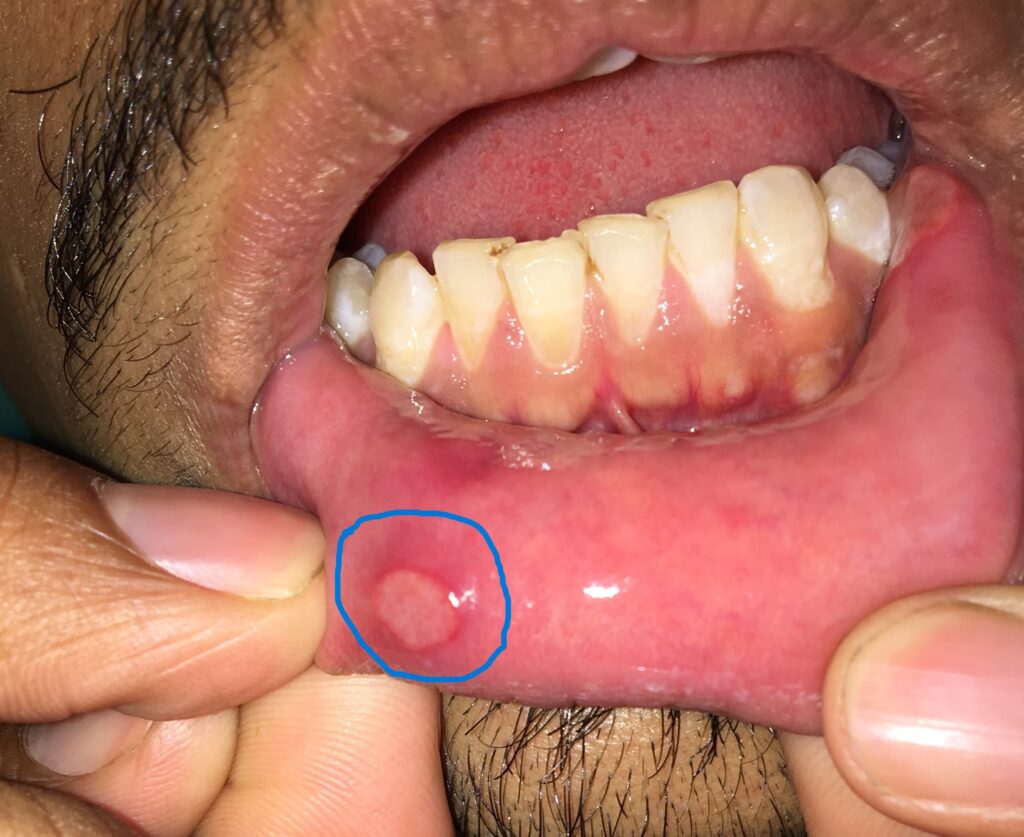
EDS can significantly impact oral health, presenting various challenges:
- Fragile Oral Mucosa: The lining inside the mouth is often thin and delicate, leading to easy bruising and tearing.
- Gum Disease: An increased susceptibility to periodontal diseases, including early-onset periodontitis, which can result in gum recession and tooth loss.
- Temporomandibular Joint (TMJ) Issues: Joint hypermobility can cause TMJ dislocations, pain, and dysfunction.
- Dental Anomalies: Abnormalities such as high cusps, deep fissures in molars and premolars, and enamel hypoplasia are common.
- Delayed Wound Healing: Post-dental procedure healing may be prolonged, with an increased risk of complications.
Investigation and Diagnosis
Diagnosing EDS involves a combination of clinical evaluation and genetic testing:
- Clinical Assessment: Evaluation of joint hypermobility using the Beighton score, skin elasticity tests, and examination of scarring patterns.
- Genetic Testing: Identification of specific genetic mutations through blood tests can confirm the diagnosis.
Prevention and General Care
While EDS is a genetic condition and cannot be prevented, proactive management can mitigate complications:
- Regular Medical Check-Ups: Ongoing monitoring by healthcare professionals familiar with EDS.
- Protective Measures: Using protective gear during physical activities to prevent injuries.
- Patient Education: Informing patients about their condition to encourage self-care and awareness.
Oral Care and Required Modifications
Dental care for individuals with EDS requires specific adaptations:
- Gentle Handling: Due to fragile oral tissues, dental professionals should use atraumatic techniques during examinations and procedures.
- Customized Oral Hygiene Plans: Developing tailored oral care routines that consider the patient’s unique needs.
- Frequent Dental Visits: Regular appointments for professional cleaning and early detection of potential issues.
- Orthodontic Considerations: Orthodontic treatments may need modification, as teeth in some EDS patients can migrate faster than expected. After positioning, prolonged use of retainers may be necessary to maintain alignment.
Instructions for Patients
Patients with EDS should adhere to the following oral care guidelines:
- Use Soft-Bristled Toothbrushes: To minimize gum damage.
- Implement Proper Brushing Techniques: Gentle brushing to avoid injuring delicate tissues.
- Floss Carefully: To prevent gum injury, consider using water flossers or interdental brushes as alternatives.
- Prevent TMJ Dislocation: To prevent jaw joint (TMJ) dislocation, avoid excessive mouth opening during activities such as yawning or dental procedures. When yawning or opening your mouth widely, support your chin with your hand to minimize the risk of dislocation.
- Maintain a Balanced Diet: Limit sugary foods and beverages to reduce the risk of tooth decay.
- Stay Hydrated: Adequate water intake supports overall health and oral moisture.
Role of Dentists and Oral Physicians
Dental professionals play a crucial role in managing EDS-related oral health issues:
- Early Detection: Identifying oral signs indicative of EDS can lead to timely diagnosis and intervention.
- Patient Education: Providing information on EDS and its oral implications empowers patients to manage their condition effectively.
- Collaborative Care: Given the multisystemic nature of EDS, dentists should work closely with other healthcare providers, including geneticists, rheumatologists, and physiotherapists, to ensure comprehensive care.
- Modified Treatment Approaches: Dental procedures, including extractions, restorations, and prosthetic work, should be adapted to accommodate the patient’s fragile tissues and potential bleeding disorders.
- Pain Management: Many EDS patients experience chronic pain, including in the jaw and TMJ. Dentists should consider non-invasive pain relief methods, such as occlusal splints or physiotherapy, before resorting to surgical options.
Conclusion
Ehlers-Danlos Syndrome (EDS) presents unique challenges in oral and dental care due to its effects on connective tissue. From fragile oral mucosa to TMJ instability and periodontal disease, the dental implications of EDS require specialized care and treatment modifications. Patients must adopt a meticulous oral hygiene routine, while dentists should employ gentle techniques, frequent monitoring, and interdisciplinary collaboration to ensure optimal outcomes. Raising awareness about EDS among dental professionals can lead to early diagnosis, improved patient care, and better long-term oral health.
Frequently Asked Questions (Q&A)
- Can EDS affect the teeth directly?
While EDS primarily affects connective tissues, some patients experience enamel defects, high palatal vaults, and increased tooth mobility. - What precautions should dentists take when treating EDS patients?
Dentists should use gentle handling techniques, avoid excessive stretching of oral tissues, and be cautious with anesthetics, as some EDS patients may have altered responses to local anesthesia. - How can EDS patients prevent gum disease?
Maintaining a diligent oral hygiene routine, including brushing with a soft-bristled toothbrush, using an antimicrobial mouthwash, and visiting the dentist regularly, can help prevent periodontal issues. - Are orthodontic treatments safe for individuals with EDS?
Orthodontic treatments can be challenging due to increased tooth mobility and slow healing. Retainers may be required for an extended period to maintain results. A specialist should assess and customize the treatment plan accordingly. - Can EDS patients undergo dental extractions or surgeries?
Yes, but with caution. Due to fragile tissues and potential bleeding issues, extractions and surgeries should be performed with minimal trauma, and sutures may be necessary to aid healing. Pre- and post-operative care should be planned meticulously. - Why do EDS patients often experience jaw pain?
EDS can lead to temporomandibular joint dysfunction (TMD) due to joint hypermobility and weak connective tissues, causing frequent dislocations, pain, and clicking sounds in the jaw. - Is there a cure for EDS-related dental issues?
There is no cure for EDS, but effective management strategies, including preventive care, pain management, and customized dental treatment, can significantly improve oral health and quality of life.
This comprehensive guide provides valuable insights into the oral health challenges associated with Ehlers-Danlos Syndrome. By understanding the condition and its impact on dental care, both patients and dental professionals can work together to ensure better oral health outcomes.