Sjogrens-syndrome (Image courtesy of Shutterstock)
Introduction
Sjögren’s Syndrome (SS) is a chronic autoimmune disorder primarily affecting the body’s moisture-producing glands, leading to dry mouth (xerostomia), dry eyes, and systemic complications. Dentists, particularly oral medicine specialists, are often the first healthcare professionals to identify signs of this condition due to its significant oral manifestations. Early recognition and intervention are crucial to improving the patient’s quality of life and preventing severe dental complications.
This article provides a structured, department-wise guide to managing oral health in Sjögren’s Syndrome, highlighting essential self-care tips, required modifications in dental treatments, and the role of various dental and medical professionals in comprehensive patient care.
Understanding Sjögren’s Syndrome and Its Oral Implications
Sjögren’s Syndrome is an autoimmune disorder that primarily targets the exocrine glands, leading to reduced saliva and tear production. It can exist as a primary condition or secondary to other autoimmune diseases, such as rheumatoid arthritis or lupus.
General Features of Sjögren’s Syndrome
- Persistent dry mouth and dry eyes
- Fatigue and joint pain
- Swelling of salivary glands
- Difficulty swallowing and speaking
- Increased dental decay and oral infections
- Burning sensation in the mouth
- Difficulty wearing dentures due to dry oral tissues
Oral Manifestations in Sjögren’s Syndrome
Patients with SS experience various oral complications due to the lack of saliva, which is essential for maintaining oral health. These include:
- Severe Dry Mouth (Xerostomia): Reduced salivary flow leads to difficulty in chewing, swallowing, and speaking.
- Increased Risk of Dental Caries: Saliva protects against bacteria, and its absence increases the likelihood of tooth decay.
- Fungal Infections (Oral Candidiasis): Dry conditions in the mouth create an environment conducive to yeast infections.
- Gingivitis and Periodontal Disease: Lack of saliva makes gums more prone to inflammation and infection.
- Dysphagia and Taste Alterations: Difficulty in swallowing and a diminished sense of taste.
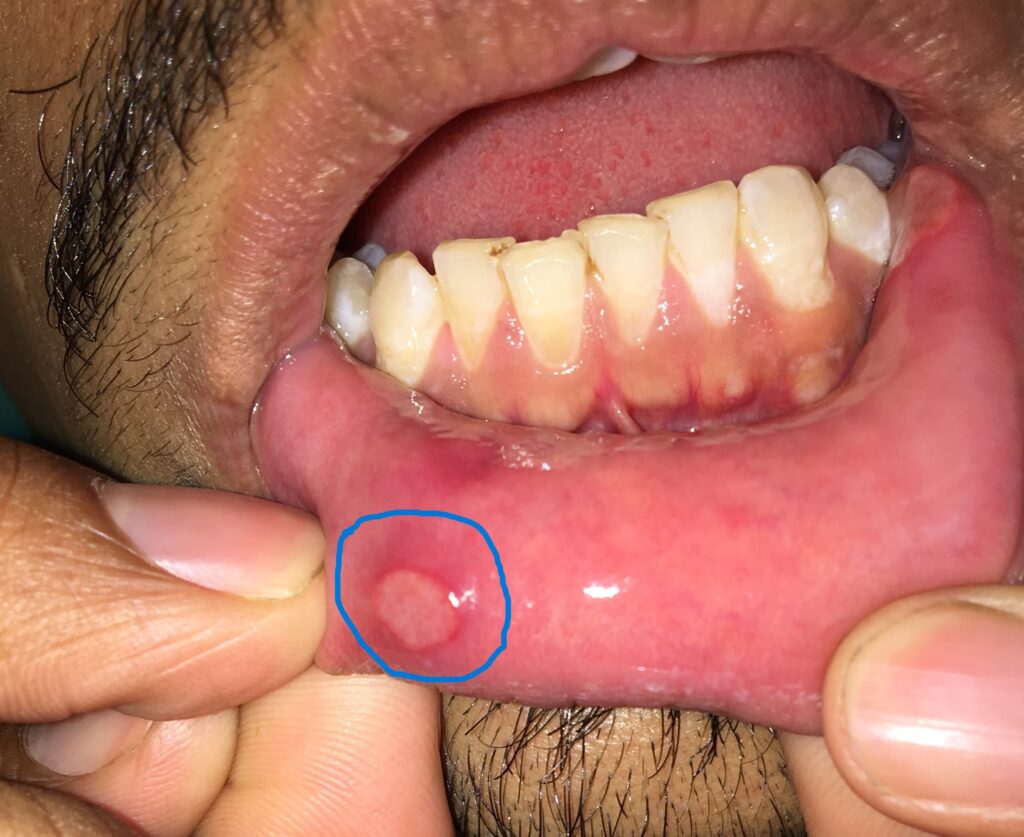
- Cracking and Sores in the Mouth: The lips and tongue may develop painful cracks or ulcers due to persistent dryness.
Diagnosis and General Care
Role of the Oral Physician
- Dentists play a vital role in recognizing early signs of SS.
- Diagnosis involves salivary flow tests, biopsy of minor salivary glands, and blood tests for autoimmune markers like anti-SSA/Ro and anti-SSB/La antibodies.
- Collaboration with rheumatologists and general physicians is essential for systemic management.
General Preventive Measures
- Regular check-ups with both dental and medical professionals.
- Hydration: Drinking plenty of water throughout the day.
- Use of Saliva Substitutes: Artificial saliva or sugar-free lozenges to stimulate salivary flow.
- Avoiding Alcohol and Caffeine: These substances exacerbate dryness.
- Maintaining a Balanced Diet: Incorporating omega-3 fatty acids and vitamin-rich foods to support immune function.
Oral Care Considerations for Sjögren’s Syndrome (Department-Wise)
- Oral Medicine & Radiology
Problems & Complications:
- Often the first department to suspect Sjögren’s Syndrome based on dry mouth complaints and oral lesions.
- Increased risk of oral candidiasis and opportunistic infections.
- Difficulty in early-stage diagnosis due to overlapping symptoms with other conditions.
Modifications Required:
- Conduct thorough salivary flow assessments and minor salivary gland biopsies if needed.
- Use antifungal treatments proactively in cases of oral candidiasis.
- Collaborate with rheumatologists and general physicians for systemic management.
Patient Oral Care Tips:
- Use saliva substitutes and frequent hydration.
- Avoid acidic, spicy, or dry foods that exacerbate discomfort.
- Report any persistent oral pain or ulcers to a dentist immediately.
- Oral & Maxillofacial Surgery
Problems & Complications:
- Increased risk of post-surgical complications due to impaired wound healing.
- Dry oral tissues make surgery and healing more complex.
Modifications Required:
- Use moisture-retaining techniques and lubricants before and after procedures.
- Minimize surgical trauma and use absorbable sutures.
- Ensure adequate hydration and saliva stimulation post-surgery.
Patient Oral Care Tips:
- Follow prescribed post-operative care meticulously.
- Use antimicrobial mouth rinses to prevent infections.
- Consume soft foods to avoid irritation.
- Periodontics
Problems & Complications:
- Higher susceptibility to gingivitis and periodontitis due to decreased saliva flow.
- Increased plaque buildup leading to rapid periodontal disease progression.
Modifications Required:
- Frequent, gentle scaling and root planing to prevent gum disease.
- Use fluoride and antimicrobial treatments to reduce infection risks.
- Recommend customized oral hygiene aids like water flossers instead of traditional floss.
Patient Oral Care Tips:
- Brush gently with an extra-soft toothbrush.
- Use alcohol-free antimicrobial mouthwashes.
- Regular periodontal check-ups to detect issues early.
- Prosthodontics & Dental Implants
Problems & Complications:
- Denture irritation due to lack of saliva.
- Delayed healing and higher implant failure rates.
Modifications Required:
- Use flexible dentures with soft liners to prevent irritation.
- Evaluate bone health and healing capacity before implant placement.
- Extended healing periods before prosthesis placement to improve success rates.
Patient Oral Care Tips:
- Keep dentures clean and moist when not in use.
- Maintain excellent oral hygiene around implants.
- Avoid excessive chewing stress on new restorations.
- Endodontics
Problems & Complications:
- Increased tooth sensitivity and susceptibility to root decay.
- Potential difficulties in achieving effective local anesthesia.
Modifications Required:
- Use desensitizing agents and fluoride varnishes to protect exposed dentin.
- Employ multiple anesthesia techniques to improve pain control.
- Reinforce endodontically treated teeth with fiber posts and durable restorations.
Patient Oral Care Tips:
- Avoid extremely hot or cold foods.
- Use prescribed fluoride toothpaste to strengthen enamel.
- Seek early intervention for persistent tooth pain.
- Orthodontics
Problems & Complications:
- Dry mouth increases plaque buildup around brackets.
- Orthodontic appliances may cause further irritation to oral tissues.
Modifications Required:
- Use low-friction brackets and moisture-friendly materials.
- Recommend frequent fluoride applications to prevent decay.
- Encourage shorter treatment plans to minimize long-term complications.
Patient Oral Care Tips:
- Rinse with fluoride mouthwash daily.
- Maintain rigorous oral hygiene practices around braces.
- Avoid hard, sticky foods that may damage brackets.
- Public Health Dentistry
Role in Sjögren’s Syndrome Management:
- Awareness programs for early detection of SS-related oral issues.
- Community education on preventive oral care strategies.
- Support groups for patients managing chronic oral conditions.
Conclusion
Sjögren’s Syndrome poses significant oral health challenges due to severe dry mouth and increased risk of dental complications. Dental professionals play a crucial role in early diagnosis, preventive care, and treatment modifications to enhance patient comfort and oral health. Patients should adopt meticulous oral hygiene routines, while interdisciplinary collaboration among dentists, rheumatologists, and general physicians is essential for comprehensive care.
Frequently Asked Questions (Q&A)
- Can Sjögren’s Syndrome cause permanent damage to teeth?
Yes, chronic dry mouth increases the risk of cavities, gum disease, and enamel erosion, leading to permanent damage if left untreated. - How can patients relieve dry mouth symptoms?
Using saliva substitutes, drinking water frequently, sucking on sugar-free lozenges, and using a humidifier at night can help. - Can dental implants be successful in patients with Sjögren’s Syndrome?
Dental implants have a higher risk of failure due to slow healing and reduced saliva production. Thorough pre-implant evaluation and extended healing times are necessary. - Is there a specific toothpaste recommended for Sjögren’s Syndrome patients?
Yes, fluoride-based, non-foaming, and alcohol-free toothpastes are recommended to minimize irritation and prevent cavities. - What are the best dental hygiene practices for Sjögren’s Syndrome patients?
Brushing twice daily with a soft-bristled toothbrush, using an antimicrobial mouthwash, and maintaining regular dental check-ups are essential. - Are there medications to improve salivary flow?
Yes, drugs like pilocarpine and cevimeline can help stimulate saliva production, but they require a doctor’s prescription. - Can Sjögren’s Syndrome cause bad breath?
Yes, dry mouth leads to bacterial overgrowth, which can cause bad breath. Maintaining oral hygiene and staying hydrated can help reduce it.